
Living with a hiatal hernia feels like going through a maze, one misstep can lead to discomfort that can derail your entire day.
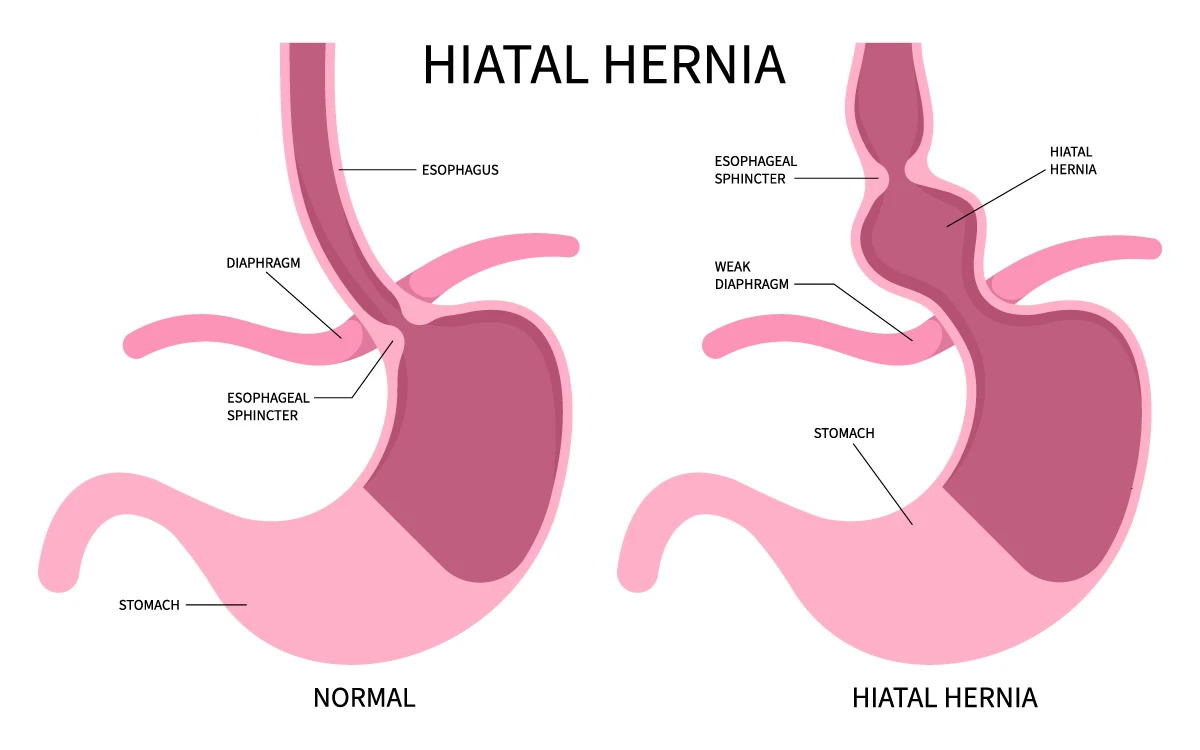
A hiatal hernia happens when the top of your stomach slips through a small opening in your diaphragm, where it’s not supposed to be. This happens when the muscles around the diaphragm weaken or get strained, allowing the upper part of your stomach to push through an opening called the hiatus. It causes a lot of bloating and in my case, many people have mistaken this inflammation attack for a pregnancy bump, especially as I rub the top of my stomach to calm it down.
.webp)
This can be caused by several factors (outside of harmful medications and eating habits), including:
When the stomach moves into this space, it disrupts the normal function of the lower esophageal sphincter (the muscle that keeps stomach acid from rising up), leading to symptoms like heartburn, acid reflux, and discomfort.
Here are my personal findings!🤓
Over the years I've made quite a lot of poor decisions that have led me to having a hiatal hernia, see previous blog post called Gut Feelings, Skin Deep. I've learned that managing this condition isn’t just about avoiding certain foods or sticking to a rigid routine. It’s about learning to listen to my body and creating an environment that supports healing. Let me take you through the lessons I’ve learned:
Routine Rumble
When I first started managing this issue I started with a disciplined approach. I tracked every meal, symptom, and trigger in a food journal, which helped me identify patterns. For instance, I realized the hiatal hernia attacks would often flare up a week before my menstrual cycle. Hormonal stress would disrupt my gut, which led to missed meals or cravings for foods that weren’t good for me.
As helpful as tracking this process was, it eventually became its own source of stress. I was so focused on getting everything “right” that I wasn’t giving my body the space to heal naturally. Over time, I learned that once I identified my triggers, it was more effective to let go of the rigidity and embrace a more intuitive approach. Now, I've learned to trust my body’s signals and eat when I’m ready, focusing on creating a peaceful environment for digestion rather than obsessing over tracking.
Rush Hour: Breaking my Fast
I used to believe that eating breakfast by a certain time would prevent gut issues later in the day. That's what I thought the pattern showed me... but sometimes we don't actually know how to read patterns. For example, if it got later than I'd normally eat, my body was likely feeling jittery from hunger, therefore I would eat something unhealthy or eat super quickly to ease the hunger. This doesn't necessarily mean that it's because I ate late, but more so because of the way I ate and the environment I ate in. I was focusing on the symptoms. So rushing through my morning and forcing myself to eat on a schedule only added stress. When you’re stressed, your body releases cortisol, the “fight or flight” hormone, which tells your body to focus on survival, not digestion. This leads to painful flare-ups.
I was so strict with myself, that when a friend shared their wisdom with me to consider fasting, I immediately rejected it by saying that would never be possible because I "needed" to eat at a certain time every day to avoid the pain. I made that agreement, so my body followed through with it. Funny enough, a few months later when I did try fasting as a last resort, it was like a reset for my gut. It really helped! It basically shifted my mindset and helped me release all the control I had about how I do things. It also supercharged my spiritual walk with Christ, because I was feeding myself the Word during that time. Win-Win!!!
So now instead of sticking to a rigid breakfast time, I simply sit down to eat once I'm able, I do so calmly and very mindfully🤭, and that has made a huge difference! God has been showing me the balance between taking control of my life (aka "Get Up and WALK"), while also surrendering to His guidance. It's a beautiful dance in all aspects of my life, including my gut health.
Digest the Moment: Multitasking Isn’t on the Menu
I used to think I could be productive by eating while working, attending meetings, or even watching a show. But I learned that splitting my attention between my food and something else led to poor digestion. For me, digestion requires focus, and when my brain is engaged elsewhere, my body can’t digest food properly.
Now, I make sure to eat in a calm, distraction-free environment, My body is sensitive to the energy around me, and creating a peaceful space for meals is essential for healthy digestion.
Gut Diversity: Everyone Eats (and Digests) Differently
It’s important to remember that not everyone's system thrives in calm environments like mine does. Some people with faster metabolisms actually digest better in busy, high-energy settings. Their bodies thrive in environments with lots of movement, like a crowded café. But for me—and others whose bodies might freeze in what it perceives as a chaotic environment—calmness is necessary.
Food with a Mood
Beyond the eating environment, I’ve also become mindful of where the food itself comes from. I’ve often turned down meals cooked by my own mother when I sensed she prepared them in a state of stress. The same goes for restaurants. I’ve walked out of places after sitting down and noticing distress among the staff or chaos in the kitchen. Food carries the energy of the environment in which it’s made, and that energy can affect digestion.
Here's the thin line though: there are some instances when I can't control my surroundings. I have to make a conscious decision to still eat even when it's not ideal for my digestion. In these cases, I have to really tap into myself. I get really grounded and breathe deeply, speak to my body and pray for God to calm me so that the external doesn't affect me internally. It's a good reminder that we can't control everything, but we can be in control of ourselves. It simply takes a little more of a conscious effort to regulate whilst in the noise.
My Go-To Gut Savers:
While avoiding triggers and creating a peaceful environment are essential, I’ve also developed specific techniques for managing flare-ups when they happen. Here’s what works for me:
- Loose clothing: I am not ashamed of unbuckling my jeans if I'm in the middle of an attack. Wearing loose, long dresses are now a part of my everyday wardrobe. People thought I was just dressing in loose clothing and dresses as a phase, but it's really for my gut health.
- Calming Music: Soft, soothing music helps me relax and encourages deeper breathing, which provides immediate relief when I feel discomfort coming on. There's a specific YouTube track that I sometimes listen to that has some frequencies that are ideal for our gut.
- Deep Breathing: Diaphragmatic breathing, also known as belly breathing, is a simple but powerful tool. By slowing down and breathing deeply, I help my body shift from “fight or flight” to “rest and digest,” allowing my digestive system to function more effectively.
- Stomach Tapping: Gently tapping on my stomach helps release trapped gas and reduce inflammation during flare-ups. It’s like nudging the stomach to get into action. In addition to this, I've found that allowing the water from the shower head to just hit my stomach also has the same effect of the manual tapping. The sound of water also is very healing, and so it allows that inflammation to subside by creating this effect that causes the trapped inflammation to move and subside.
- Yogurt for Gut Balance: A high-quality probiotic yogurt is a lifesaver when the hiatal hernia is in full attack mode. It helps restore good bacteria, calming my system and aiding digestion.
- Gratitude and Prayer: This is the most important. Pray and thank God WHILE in the pain. This has strengthened our relationship. People usually will pray for healing of their pain, and while I do this as well, there's a different layer we often miss. I often lay and ask for God to be with me while the pain subsides. From experience I know that this pain is temporary and I will be able to feel normal after a while. I'm reminded that the God who is with us (Emmanuel), is no stranger to pain, and there is so much on the other side of our physical pains in this world. While this may not help others while experiencing debilitating pain, it has been a source of peace for me, redirecting my focus on hope.
Foods To Avoid:
I’ve learned that certain foods are major triggers for my symptoms, including:
- Tomatoes and tomato-based products (BBQ sauce, ketchup)
- Red onions
- Citrus fruits (lemons, oranges, pineapples)
- Chocolate
- Coffee
- Spicy foods
- Corn
I haven’t cut these foods out entirely. There's more context to consider. Instead of re-introducing that rigid approach and completely avoiding these foods, I focus on how and when I eat them. For example, it's best to always start with a salad or vegetables first—aka cushioning the stomach—so I pack on the fibre, which doesn't spike my insulin levels. Doing this allows my body to handle small amounts of these trigger foods. I don't believe in life-time allergies or intolerances. Over time I've re-introduced certain things back into my diet (like dairy), and have been able to tolerate it once again. Our bodies are intelligent and knows what it needs, when it needs it, and simply rejects what our system cannot support at the time.
Being rigid leaves no room for flexibility, and too much flexibility leaves no room for stability. Balance is the key to sustainable healing.
If I Nurture My Gut, Then Healing Follows
At the end of the day, healing isn’t just about avoiding certain foods or following a strict routine, it’s about creating an environment that allows your body to thrive. As I’ve learned to listen to my gut and care for my body, I’ve realized that it’s not just about finding physical relief—it’s about cultivating peace, patience, and self-control, which are all fruits of the Spirit (Galatians 5:22-23). These fruits guide me through the ups and downs, helping me practice kindness toward myself, gentleness in my approach, and faithfulness in trusting the process.
The Bible reminds us in Proverbs 14:30, “A heart at peace gives life to the body.”
Self-Reflection Prompts
.png)
- How does your eating environment affect your digestion? Do you thrive in busy surroundings, or does your body need calm and quiet?
- Are there foods that trigger your symptoms? Have you noticed a pattern in how and when you consume these trigger foods?
- How does stress impact your eating choices and digestion? What can you do to create a more peaceful eating experience?
Disclaimer: I’m not a medical doctor, just a gut enthusiast sharing my personal journey! For any serious concerns, please consult a healthcare professional—because while I may know my way around a food journal, I don’t have a PhD in digestion. 😊 Listen to your body and your doctor (that is if your doctor isn't just pumping you with meds without considering all other factors......please be discerning).












